Understanding Claim Life Cycles
A scheduled integration pulls invoiced orders from AcuityLogic POS and converts each invoice into a claim that appears in AcuityLogic Billing. Depending on your settings in AcuityLogic Admin, claims first appear in AcuityLogic Billing as On Hold or Ready to Bill.
When a claim first appears in AcuityLogic Billing, review the claim and edit it if necessary. After reviewing the claim, set the status to Ready to Bill. If your system is set up to bill VSP or other supported carriers automatically, all claims for those carriers with the status Ready to Bill are then billed to their corresponding carriers.
If your system is not set up to bill claims for specific carriers automatically, review claims for those carriers and change their statuses to Ready to Bill when you are ready to bill the claims. Unless you are billing claims through TriZetto or to VSP or a supported carrier automatically, print the CMS 1500 forms for the claims and mail the forms to the appropriate carriers. If you are sending claims for carriers through TriZetto, bill those claims from the Billing Claims - GatewayEDI Transmission window in AcuityLogic Billing.
After a carrier pays the balance of the claim, record the payment in the Process Payments module. After the complete outstanding receivable for a claim is paid and recorded in AcuityLogic Billing, the claim status changes to Fully Paid. If a carrier rejects a claim, you can edit the claim and resend it to the carrier, bill the claim to the patient, or write off the claim. Record all payments from patients in the Process Payments module.
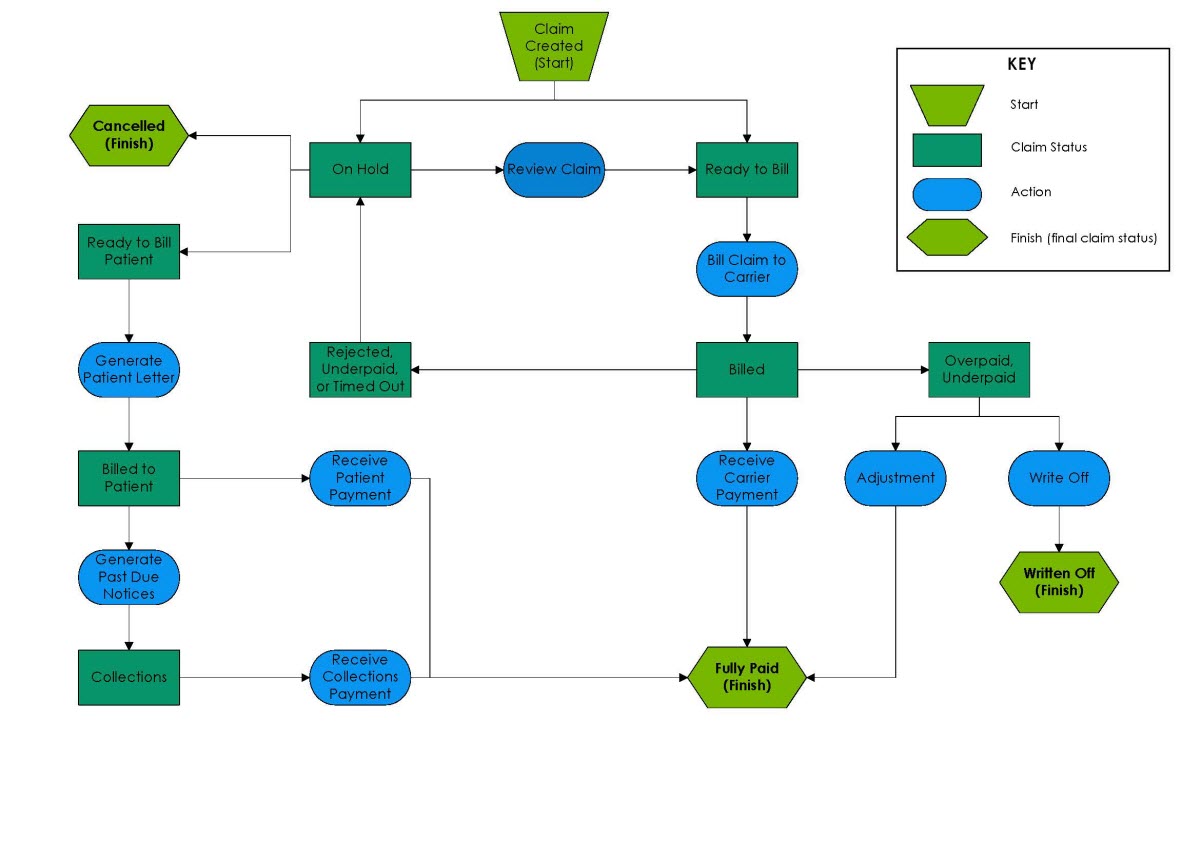
The following flowchart explains the claim life cycle in terms of claim statuses.