What's New in AcuityLogic 8.3 for Cloud Users
Eyefinity announces the newest version of AcuityLogic. In addition to resolving known issues in previous versions of AcuityLogic, this updated version offers new features and expanded functionality.
Topics include the following:
For more information on AcuityLogic features, training, and integrations, contact your account representative, or call Eyefinity at
BackOffice Enhancements
BackOffice includes an enhancement in the following area:
Generating the Sales Report by Vision Plan Report
AcuityLogic for Cloud and AcuityLogic for Pearle Vision users can now generate the Sales Report By Vision Plan (AC121) report.
Billing Enhancements
Billing includes enhancements in the following areas:
Identifying Manual or Automatic Billing for EDI Claims
Previously, when the system or a user billed a claim to a carrier through TriZetto (formerly Gateway EDI), thereby changing the claim's status to Billed, "System" always appeared in the Employee column of the Claim History table in the Claim Detail window. Now, the name of the logged-in users appears in the Employee column, enabling you to easily identify whether the claim was billed manually by a user or automatically by the system.
Improving the Performance of EDI Claim Submissions
The speed at which AcuityLogic generates and submits EDI claims to TriZetto is greatly improved. For example, 200 claims were previously processed in 8 minutes. Now, 200 claims are processed in 2.5 minutes.
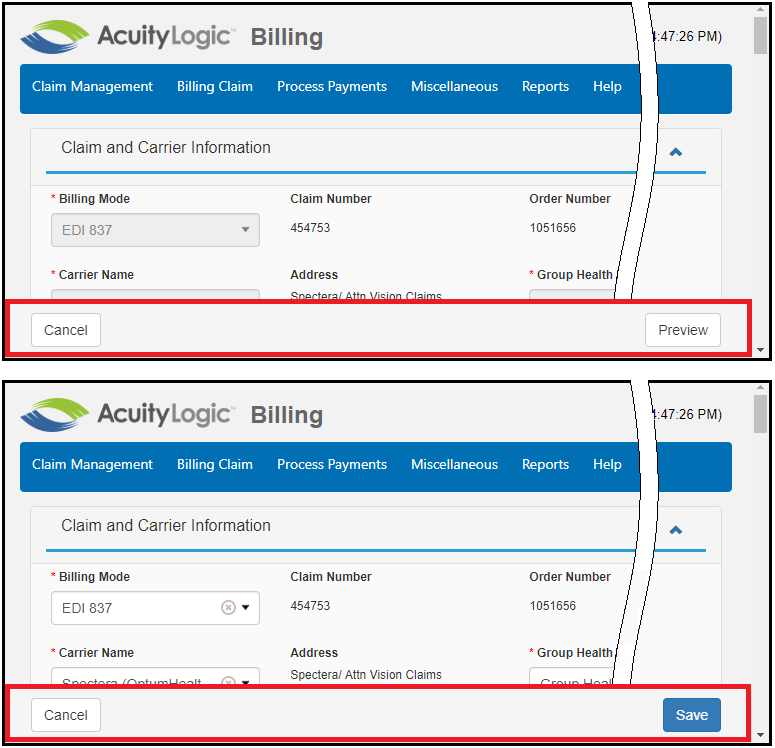
Keeping Claim Preview and Save Bars Visible
The Preview bar in the View Claim window and the Save bar in the Edit Claim window now remain visible at the bottom of the window as you scroll:
System Enhancements
In AcuityLogic 8.3, performance in several areas of POS operations was significantly improved.
Fixed Issues
AcuityLogic 8.3 fixes issues in the following areas:
Admin
- When you unmap a contact lens style for any company and then save your change, an unknown error no longer occurs.
Billing
- In the Edit Claim window, the Insured's ID Number (Box 1a) and Other Subscriber ID (Box 9) fields are no longer case sensitive, and their contents are always saved in uppercase letters, regardless of the case the user enters. This prevents TriZetto from rejecting claims because they contain lowercase letters in the subscriber's primary ID.
- When you select Print New CMS Form (Version 02/12) from the Action drop-down list for a claim in Ready to Bill status in the Claim Management window, the claim's status now changes to Billed.
- Unpaid claims that are edited after their status is changed to Billed are now marked Timed Out after 60 days unless the edit changes a receivable. In that case, the edited line item is set to Ready to Bill and must be manually changed to Billed, which resets the claim’s billed date to the date of the manual change.
POS
- When you apply an insurance plan that has a miscellaneous dispensing fee to an order in the order pricing window, the fee is now applied only once, even if you remove and reapply the insurance multiple times. In addition, you can now easily remove a miscellaneous fee in POS by clicking the fee's delete icon (
 ). Previously, another miscellaneous dispensing fee was added each time you reapplied the insurance, and you could remove duplicate instances of the fee from the order only by editing the claim in Billing.
). Previously, another miscellaneous dispensing fee was added each time you reapplied the insurance, and you could remove duplicate instances of the fee from the order only by editing the claim in Billing. - When you try to save VSP insurance benefit calculations in the VSP Calculation window, you no longer receive an error message if the sum of a line item's Patient Responsibility, Patient Copay, and Insurance Reimbursement amounts exceeds the item's retail amount. Instead, the calculation is successfully saved.
- In the Patient Insurance Balance Payments window, you can now make partial payments on insurance balances. Previously, you could not click Complete Payment if the total of all payments added to the Payments table did not equal the total insurance balance.
- If you apply an insurance plan with the Material Allowance and Allow Package Discount special option methods to an order that includes a package discount, the material allowance is now applied to the remaining balance of the order after the package discount is applied. Previously, the package discount was removed when an insurance plan with a material allowance was applied, and the allowance was then applied to the order's full retail price.
- When you void an order whose frame status/source is Provided By, the frame's on-hand quantity in inventory no longer increases.
- If an order contains a package, the package information—including its name and discounts—now appears on the order's invoice. Previously, that information was omitted from the invoice, which prevented patients from verifying the accuracy of the order's calculations and which caused errors in the Daily Office Flash Sales report (AC112).
- If a patient is a Child/Dependent of an insurance subscriber and the subscriber does not exist in your AcuityLogic system, the Responsible Party value in the patient's Profile > Other Information tab is no longer overwritten by the subscriber's name when you add the subscriber's plan to the Insurance tab of the patient's profile.