Posting Payments to Claims
This section explains how to post payments to claims in AcuityLogic Billing.
Topics include the following:
An internal claim is a claim created in AcuityLogic and billed through AcuityLogic Billing. Unless you recently moved from another billing system, all received payments will be for internal claims.
- Open the Carrier Checks or Patient Checks window for a claim, expand the Related Claims panel, and display the search options.
See Opening and Navigating the Carrier and Patient Checks Windows.
- In the Related Claims panel, enter the claim details.
- Click Search.
The claims that meet your search criteria are displayed.
- To specify whether the payment overpays or underpays the claim, click the +/- icon in the row of the claim.If the payment fully pays the claim, click the Full icon. AcuityLogic applies the payment to the claim, and the claim appears in the Payment Detail panel.
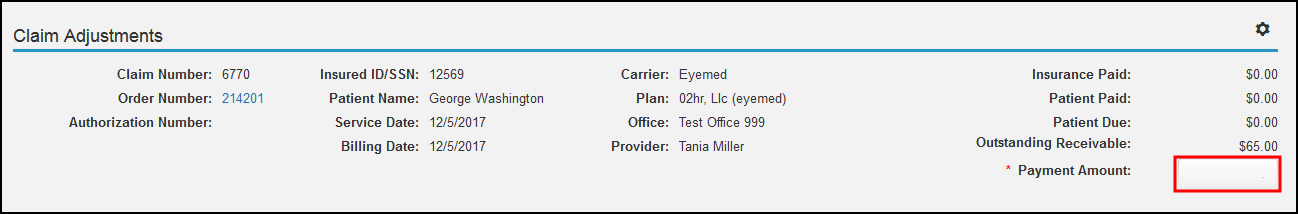
The Claim Adjustments window opens.
- In the upper-right corner of the window, click the Settings icon (
 ) to select the following options:
) to select the following options:- Pre-Populate Payment Amount to populate the line item Payment Amount fields for the claim automatically.
- Auto Adjustment to enable automatic adjustments for line items. You can perform only one automatic adjustment per claim.
- To save the settings for the current user, click Save. They can be changed later.
- In the Payment Amount field in the upper section of the window, enter the total amount paid toward the claim.
- In the Payment Amount field for a line item, enter the amount paid towards the item.
- If you selected the Pre-Populate Payment Amount check box in step 6, the field is prepopulated, and you can make changes as needed.
- If you selected the Auto Adjustment check box in step 6, click the Automatically adjust line item icon to have AcuityLogic make an automatic adjustment.
The Adjustment Type and Comment fields appear under the line item.
- From the Adjustment Type drop-down list, select an adjustment type for the line item.
- In the line-item adjustment's Amount field, enter the amount of the adjustment.
- (Optional) In the Comment field, enter a note about the adjustment.
- To record another adjustment for the line item:
- Click + Add More.
- Repeat steps 9–12.
Each line item can have three adjustments.
- Click Save to save your changes and close the Claim Adjustments window.
The following table describes the adjustment types:
| Adjustment Type | Description |
|---|---|
|
Adjustment |
Performs an adjustment to the line item similar to adjustments made in the Claim Detail window. Enables you to change the outstanding receivable. Depending on the final outstanding receivable amount, the adjustment changes the line item status to Underpaid, Fully Paid, or Overpaid. |
|
Bill to Insurance |
Transfers the specified receivable amount to a secondary insurance carrier and creates a claim. The receivable of the original line item is adjusted by the transfer amount and entered as the receivable for the line item on the new claim. |
|
Bill to Patient |
Transfers the amount in the Remaining column from the carrier to the patient. Performs the same action as clicking the Ready to Bill Patient button in the Claim Detail window. |
|
Biller Review |
Adds a marker to indicate that another biller needs to review the claim after the payment is applied. |
|
Rejections |
Changes the line item status to Rejected if the payment amount is $0. |
|
Write Off |
Performs a write-off to the line item similar to write-offs in the Claim Detail window. Enables you to change the outstanding receivable. Changes the line item's status to Written Off. |
The claim appears in the Payment Detail panel.
An external claim is a claim billed through another billing system. If you recently moved to AcuityLogic Billing from another billing system, follow this procedure to post payments to an external claim.
- Open the Carrier Checks window for a claim, and expand the Related Claims panel.
See Opening and Navigating the Carrier and Patient Checks Windows.
- Click Post External.
- In the Post External Claim Transactions window, record the details of the claim in the available fields.
- Click Post Transaction.
The external claim appears in the Payment Detail panel.