Adding Eligibilities Using the TriZetto Integration
If your practice has TriZetto integrated with Encompass, you can now obtain patient eligibility information for TriZetto insurance payors automatically. This feature eliminates the need to access TriZetto's website to verify eligibilities.
An additional fee is required. For more information about TriZetto Provider Solutions and how to sign up for the integration, go to www.trizettoprovider.com/eyefinity.
Before you can use the integration, you need to perform the following company and office setup tasks in Administration:
- Make sure your office claims information setup is complete, including Billing NPI number.
- Enable electronic claim submission for the insurance carriers.
- Set up the third-party billing integration.
- Enter your Office Site Key.
Click here to watch a video on how to perform these setup tasks.
Additional requirements for pulling eligibilities from TriZetto:
- The patient's name, date of birth, and gender in Demographics and the subscriber information and Insured ID in Edit Insurance must match what the insurance company has on file.
- A provider must be assigned to the patient in Demographics. The provider must be subscribed to TriZetto and credentialed with the insurance carrier.
- If the provider is credentialed with the insurance carrier with a group NPI
 National Provider Identifier number. A unique 10-digit identification number required for all healthcare providers in the United States. number, you must make sure the group NPI details are recorded correctly for the insurance carrier and provider in Provider Setup. For instructions, see Setting Up Provider Insurance Details for Individual Carriers.
National Provider Identifier number. A unique 10-digit identification number required for all healthcare providers in the United States. number, you must make sure the group NPI details are recorded correctly for the insurance carrier and provider in Provider Setup. For instructions, see Setting Up Provider Insurance Details for Individual Carriers. - Some insurance plans, such as MediCal, require a legacy provider ID number or PIN to retrieve eligibilities. Enter this number in the Legacy ID field in the provider's Insurance Details window in Administration. For instructions, see Setting Up Provider Insurance Details for Individual Carriers
- On the left side of the Demographics screen, under Insurance, click Eligibility/Authorization.
- Locate the insurance plan to which you want to add eligibilities.
- Click +Eligibility. If the plan is not listed, see Adding Non-VSP Insurance Information.
The system imports the patient's insurance coverage information available from TriZetto and displays it in the Eligibilities window. The TriZetto logo in the upper-right corner of the window indicates that the information was obtained from TriZetto. The date the information was imported is also shown.
If the patient's information in Demographics does not match the information the insurance carrier has on file, or the provider is missing or not valid for TriZetto or the insurance, a warning message appears when you click +Eligibility. In the message window:
Click Correct to correct the information.
Click Continue to enter the coverage information manually without using TriZetto.
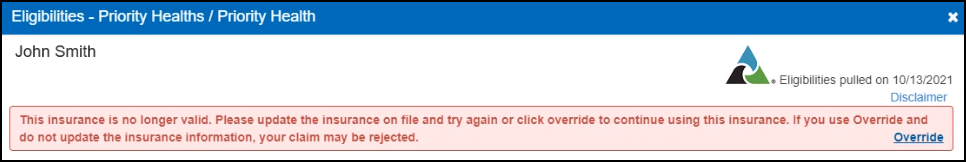
If the "This insurance is no longer valid" error message displays, see Overriding the "This Insurance is No Longer Valid" Error Message.
- Check Coverage and Claim Details and edit, as necessary. Some information may not have been available for import from TriZetto.
- Click Save.
The eligibility is added to the Eligibility/Authorization screen.
Editing Eligibilities from TriZetto
- In the Eligibility/Authorization screen, locate the eligibility you want to edit.
- Click the icon in the Eligibility column.
- Edit the Coverage information and Claim Details, as necessary.
- Click Save.
The Eligibilities window opens.
Overriding the "This Insurance is No Longer Valid" Error Message
If the "This insurance is no longer valid" error message displays in the Eligibilities window, you can override it and enter the eligibility manually instead of using TriZetto.
-
Click the Override link in the red message box.
-
Enter the eligibility information, as necessary.
-
Click Save.