Overriding Billing
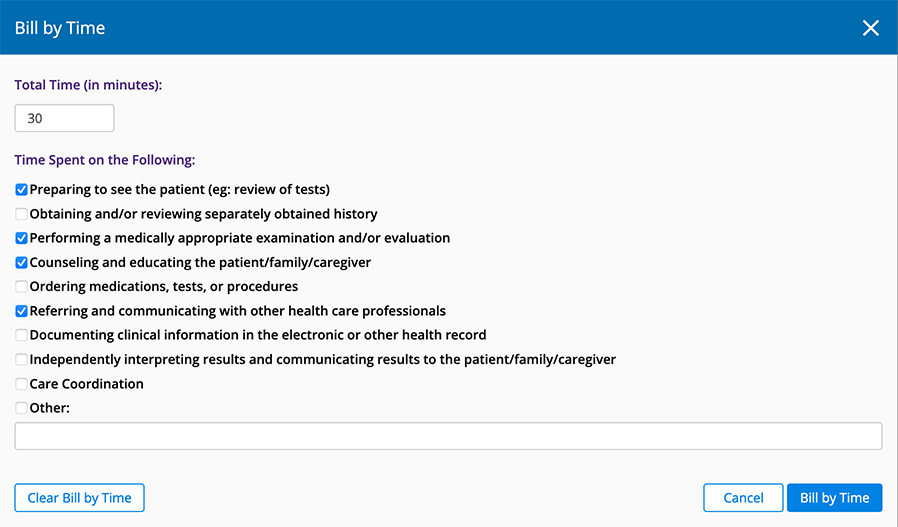
You can override a suggested billing code, bill a visit based on time, or override the entire bill including procedure codes![]() The insurance and medical industries apply universally accepted coding systems to ensure the standardization of definitions and charges. These include: CPT Codes, CPT Category II codes, DRG codes G-codes, ICD 10 codes, S-codes., CPT codes
The insurance and medical industries apply universally accepted coding systems to ensure the standardization of definitions and charges. These include: CPT Codes, CPT Category II codes, DRG codes G-codes, ICD 10 codes, S-codes., CPT codes![]() Current Procedural Terminology. The numeric codes that are submitted to insurers for payment. Every billable procedure has its own individual CPT code., modifiers, and units. This topic describes how
Current Procedural Terminology. The numeric codes that are submitted to insurers for payment. Every billable procedure has its own individual CPT code., modifiers, and units. This topic describes how
- Open the Visit Overview.
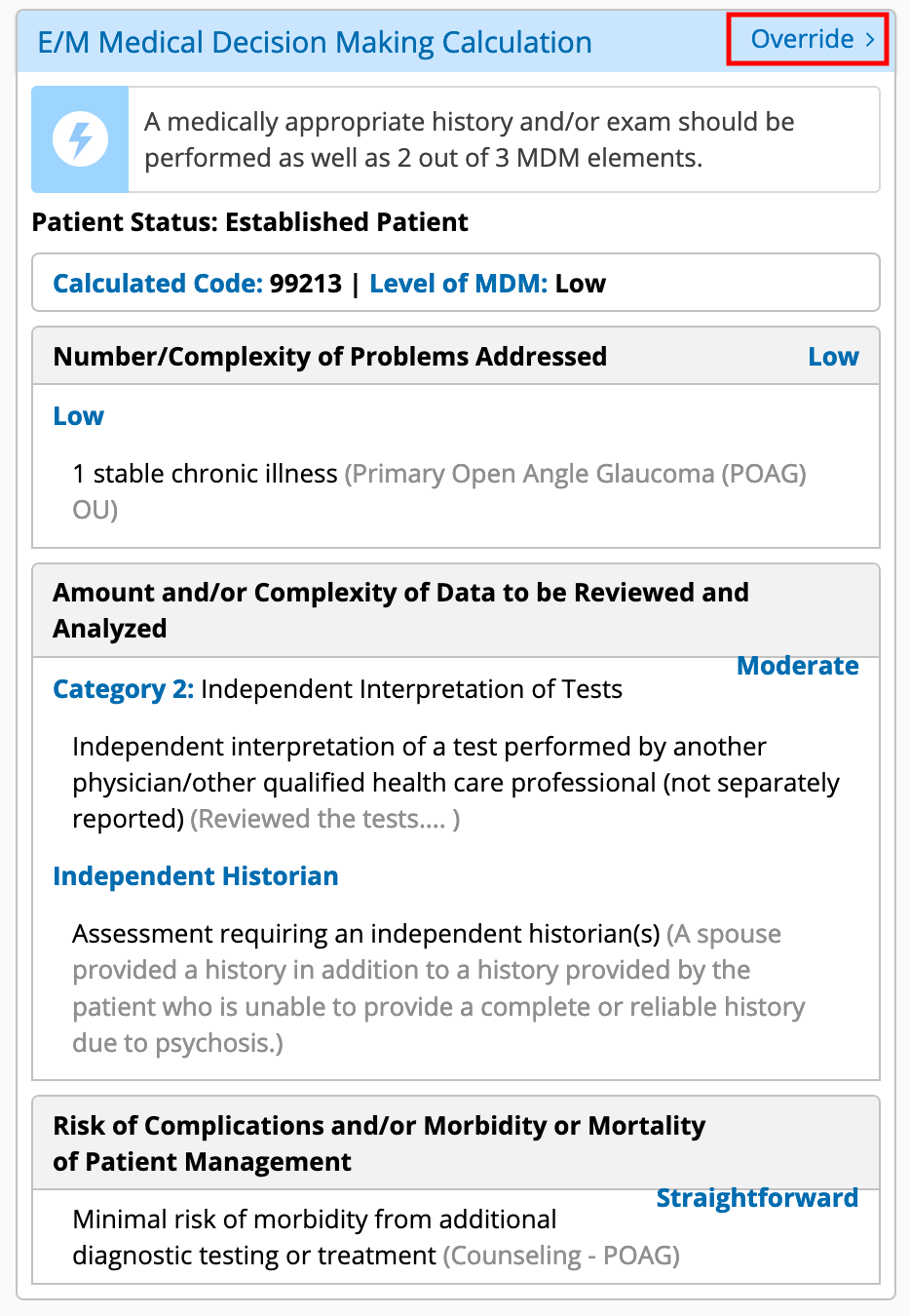
- Scroll down to the E/M Medical Decision Making Calculation section (located on the left side of the page) and click Override.
- Review the MDM calculations.
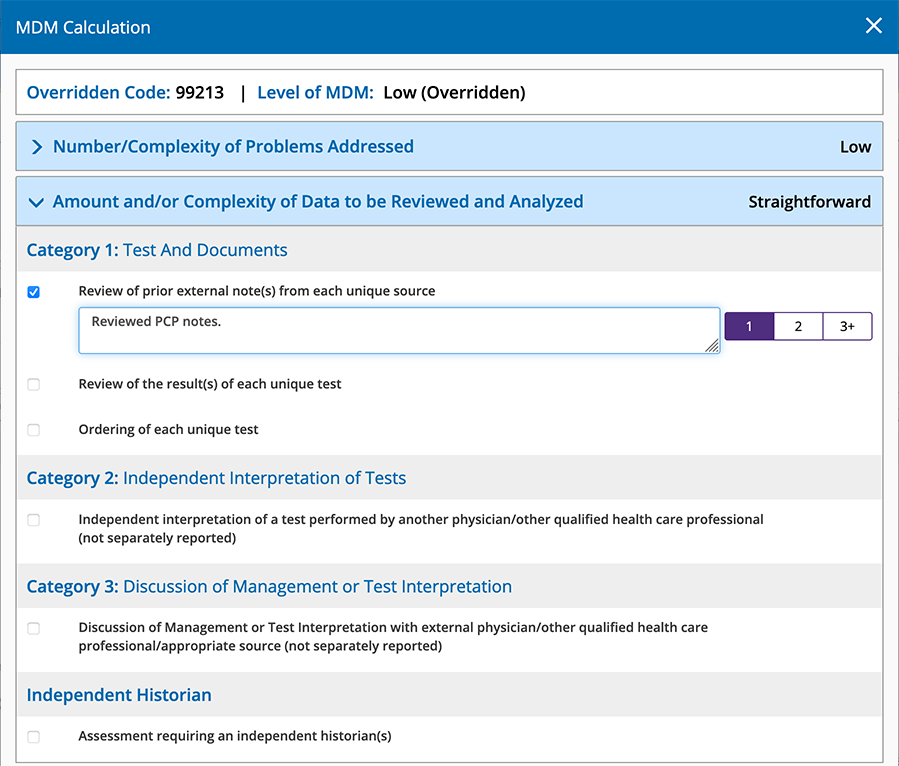
- To override a criteria, select the appropriate radio button and enter any notes.
Certain elements will prompt you to select 1, 2, or 3+. Select the number that corresponds to the number of documents from unique sources reviewed in relation to the visit.
Criteria highlighted in yellow were automatically calculated by Encompass. When you override a criterion, the highlighting is removed.
- Click Override MDM when you’re finished.
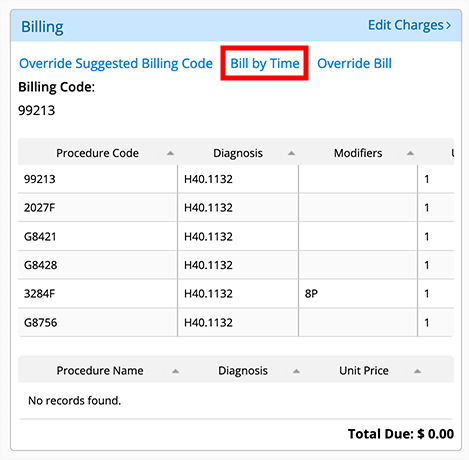
- Access the Visit Overview screen.
- Scroll down to the Billing section.
- Click Override Suggested Billing Code.
- Select the billing code you want to use from the drop-down list.
- Click Override Code to override the billing code or click Clear Override to cancel.
The Visit Overview screen appears and shows the billing code you selected.
- Access the Visit Overview screen.
- Scroll down to the Billing section.
- Click Override Bill.
The Override Bill screen appears.
- In ICD-10, click Clear to remove an ICD-10 Code
 Codes for the International Statistical Classification of Diseases. A standardized set of codes gives to every diagnosis, description of symptoms and cause of death attributed to human beings. ICD-10 is the current standard in the United States., or enter the ICD-10 Code you want to use.
Codes for the International Statistical Classification of Diseases. A standardized set of codes gives to every diagnosis, description of symptoms and cause of death attributed to human beings. ICD-10 is the current standard in the United States., or enter the ICD-10 Code you want to use.If you want to change the order of the ICD-10 Codes, use the arrows to the left of the code.
- In CPT Code, click Clear to remove the row for a CPT Code, or enter the CPT Code you want to use.
- Enter the Modifiers, Diagnosis Pointers, and Units.
- (Optional) Select the insurance you want to bill.
If you make a mistake and want to start over with the original codes, click the Reset to Calculated From Visit button. Your changes are deleted and the ICD-10 and CPT codes are populated based on the codes from the exam.
- To override the billing codes, click Override Code.
To cancel, click Cancel.
The Visit Overview screen appears and displays your changes.