Using the VSP Interface
This section describes how to handle error and warning messages you may see when you calculate benefits and submit orders and claims through the VSP interface.
This section includes the following topics:
- Understanding Error and Warning Messages
- Viewing Error and Warning Messages
- Acknowledging Warnings in Claims Management
Understanding Error and Warning Messages
While submitting VSP orders and claims through the VSP interface, you may encounter two types of messages: errors and warnings. This section explains the difference between these two types of messages. For a list of all the error and warning messages, along with explanations and examples, see Warnings and Errors in the VSP Interface.
This section includes the following topics:
To watch a video about the error and warning messages, see Understanding Claim Errors and Warnings [video]. For information on how to view the messages, see Viewing Error and Warning Messages.
Errors
Errors are distinguished by the word Error. Errors reflect conditions that must be corrected before the order or claim can be submitted. You must correct the error or the message will display again when you attempt to retransmit the order or claim.
Warnings
Warnings are distinguished by the word Warning in the message. For warnings, you have the option to edit the order or claim, or acknowledge the issue and continue with the order or claim as it is. For instructions on how to acknowledge a warning and submit the claim without making any changes to the order or claim, see Acknowledging Warnings in Claims Management.
Viewing Error and Warning Messages
Error and warning messages are displayed in the Order Status window in Material Orders and the Claim Note window in Claim Detail.
- Viewing Error and Warning Messages in Material Orders
- Viewing Error and Warning Messages in Claims Management
Viewing Error and Warning Messages in Material Orders
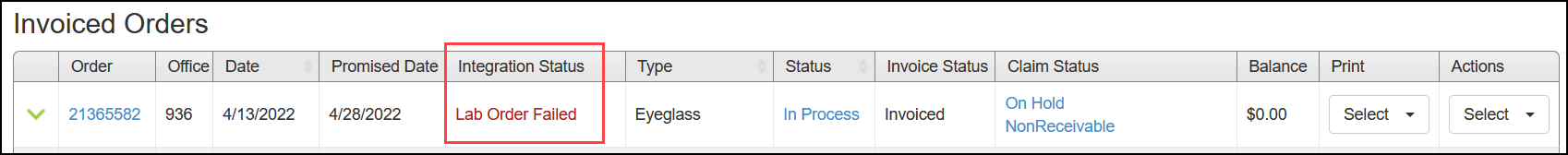
In Material Orders, VSP orders on hold due to errors or warnings are indicated with the words "Lab Order Failed" in red, displayed in the Integration Status column in the Invoiced Orders grid.
- In Material Orders, click the Invoiced tab, if it is not already displayed.
The Invoiced Orders grid lists the patient’s invoiced orders. The Integration Status column displays a message for each order that was submitted electronically.
- Lab Order Submitted means the order was successfully transmitted to the lab and the claim was successfully submitted to VSP.
- Lab Order Failed means there is a problem with the order or the integration and the order was not transmitted to the lab and the claim was also not submitted to VSP.
- Locate an order in the list and click the green arrow next to the order number.
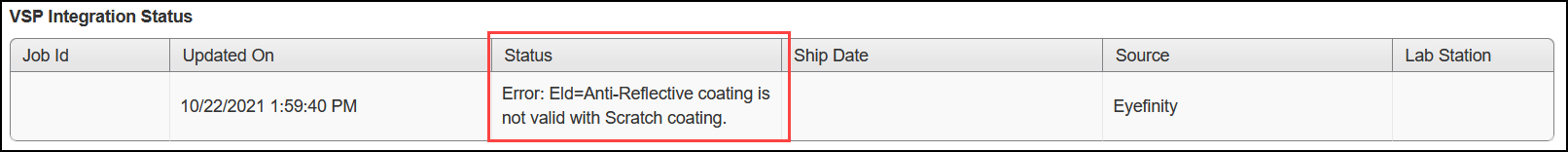
- Click the VSP Integration Status tab. The tab shows the Job ID, Updated On date, Status, Ship Date, Source, and Lab Station information. If the order failed, the panel shows the failure error or warning message instead of the Status. See Errors and Warnings for more information on the messages.
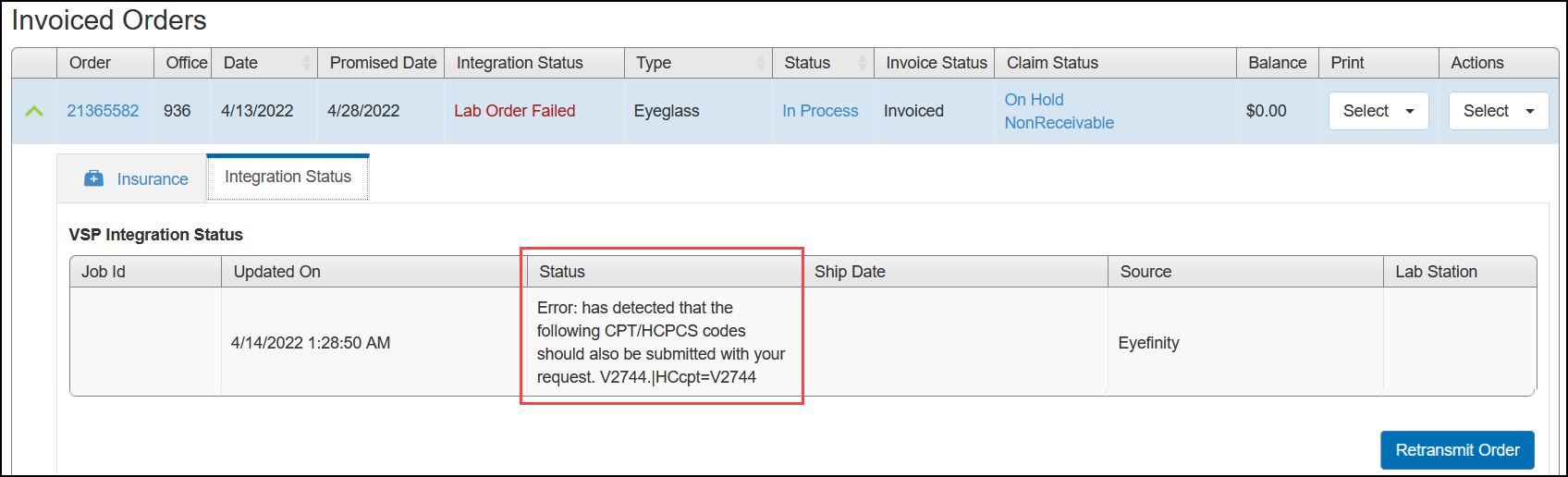
- To try sending the order again, click Retransmit Order. If the order has an error preventing it from being sent, you should fix the error before retransmitting.
Viewing Error and Warning Messages in Claims Management
You can view errors and warnings affecting a claim in the Claim Detail screen.
- In Material Orders, locate the invoiced order associated with the claim that contains the error or warning and copy the order number.
- Go to Claim Management, and use the order number to search for the claim.
- Click the Claim # link to open the Claim Detail screen.
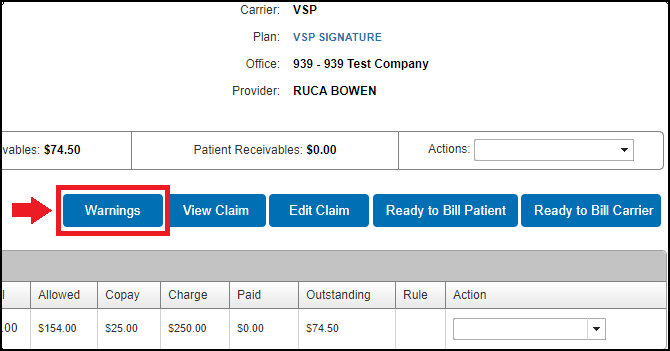
If the claim has warnings, the new Warnings button appears in the Claim Detail screen. For more information on the Warnings button, see Acknowledging Warnings in Claims Management.
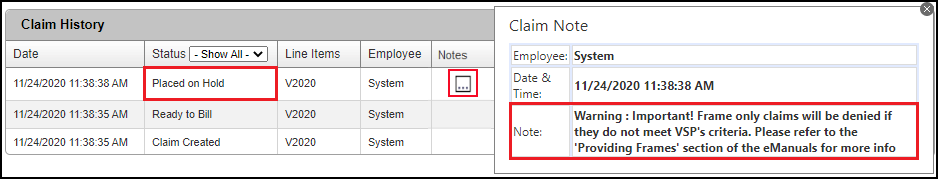
- In the Claim History list, locate the Placed on Hold line item and click the icon in the Notes column.
The Claim Note window opens, and displays any errors and/or warnings that are causing the claim to be on hold. See Errors and Warnings for more information on the messages.
Acknowledging Warnings in Claims Management
Ideally, you should fix all problems with a claim before submitting it. However, if a claim is on hold due to warnings, you can simply acknowledge them and take the claim off hold so it can be submitted.
- Open the Claim Detail window for the claim and check to see if it has warnings:
- If the claim is on hold because of a warning, the new Warnings button appears.
- In the Claim Note window, warnings are indicated by the word Warning in the Note field.
- Click the Warnings button.
The Warnings window opens.
- In the Ack column, select the check box(es) of the warning(s) that you want to acknowledge but not resolve, and then click Save.
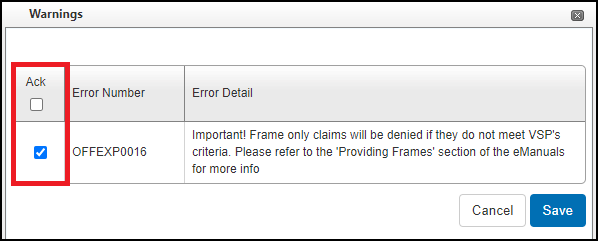
- Click Ready to Bill Carrier.
The next time the billing integration runs, the claim will be billed.